Dysautonomia + Bodywork - What’s Our Role?
IMAGE CREDIT: thedysautonomiaproject.org/
How Theory and Techniques Meet in the Treatment Room
I have been seeing more and more folks coming into the clinic with either a diagnosis of dysautonomia or a symptom set that fits the dysautonomia picture. Dysautonomia is not a “medical diagnosis”, it is a grouping of symptoms that indicates underlying autonomic nervous system disorder. The actual cause may remain a mystery but treatment can follow the specific presentation of each individual case. This is where our skills as bodyworkers can be supportive for those with these symptoms.
Defining Dysautonomia
The definition of dysautonomia can be a little slippery because the autonomic nervous system is involved in almost everything our body does without our conscious participation, like blinking our eyes or adjusting how sound is interpreted or how temperature is regulated and so on.
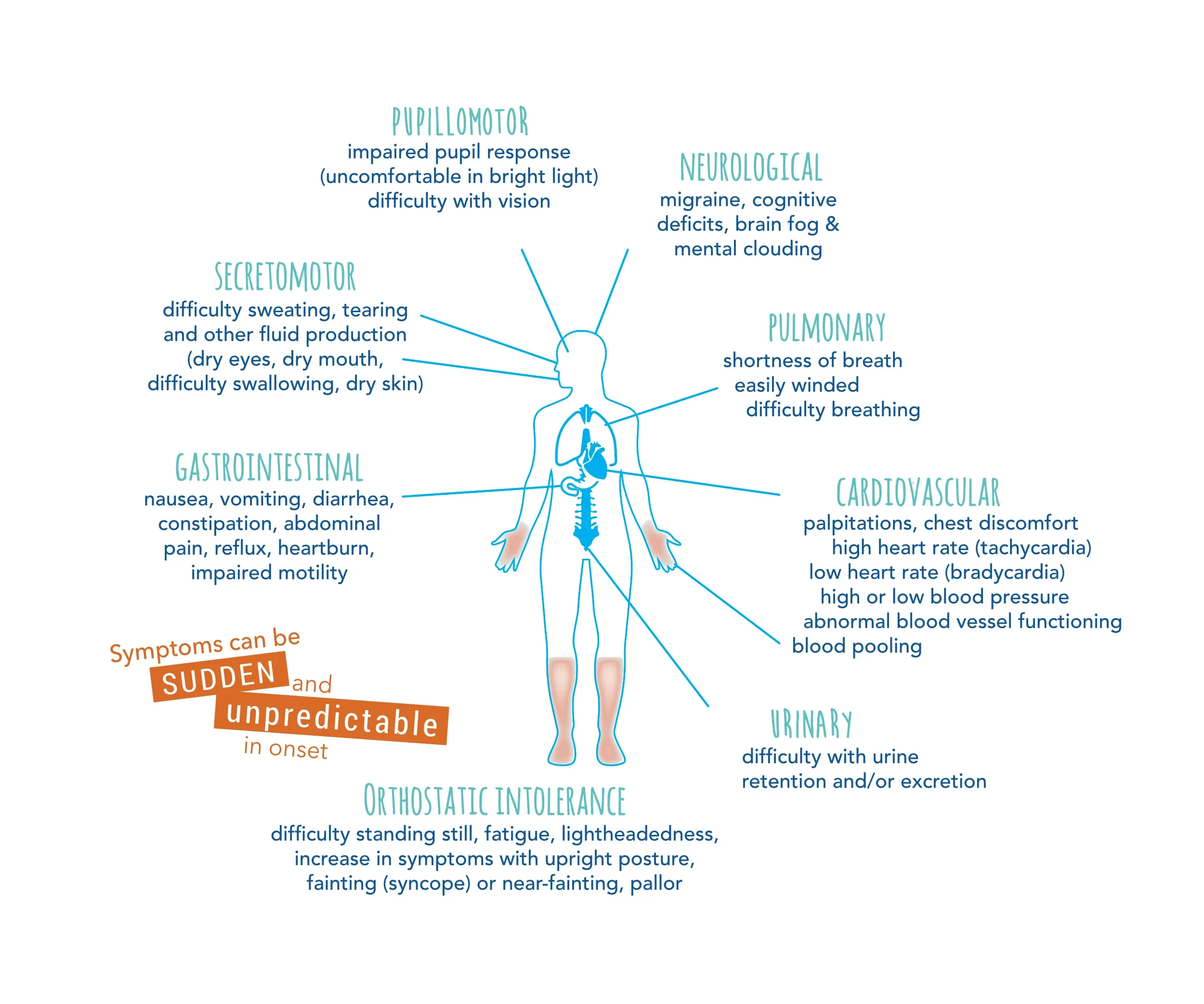
Because each body is unique, the specific presentation of autonomic nervous system issues is entirely unique to the individual. The Dysautonomia Project offers a good grouping of systems and examples of symptoms:
Neurological Symptoms: migraines, other types of headaches, cognitive deficits, brain fog and mental clouding.
Orthostatic Intolerance Symptoms: difficulty standing still, fatigue, lightheadedness, increase in symptoms with upright posture, fainting (syncope) or near-fainting, and pallor. This is commonly diagnosed as Postural Orthopedic Tachycardia Syndrome (POTS). This is one of the most common clinical presentations of dysautonomia.
Pulmonary Symptoms: shortness of breath, easily winded, and difficulty breathing.
Cardiovascular Symptoms: palpitations, chest discomfort, high heart rate (tachycardia), low heart rate (bradycardia), high or low blood pressure, abnormal blood pressure functioning, and blood pooling.
Urinary Symptoms: difficulty with urine retention and/or excretion.
Gastrointestinal Symptoms: nausea, vomiting, diarrhea, constipation, abdominal pain, reflux, heartburn, and impaired motility
Secretomotor Symptoms: difficulty sweating, tearing, and other fluid production (dry eyes, dry mouth, difficulty swallowing, dry skin).
Pupillomotor Symptoms: impaired pupil response (uncomfortable in bright light) and impaired vision.
This list does not include fatigue as a symptom. However, many of the above categories will produce pronounced fatigue. An elevated heart rhythm over time is exhausting, for example. Low blood pressure can make one both exhausted and feeling on edge (tired and wired). Chronic brain fog is exhausting. You get the idea.
Some of you may be screaming, “This is Ehlers Danlos Syndrome (EDS) or Hypermobility Spectrum Disorder (HSD)!” Maybe. In my experience, it’s helpful to focus on the symptoms presenting both specifically and as a gestalt or grouping before categorizing the symptoms diagnostically. We can get there and we don’t need to rush. Pace makes space. In some cases I think it’s important to pursue an HSD diagnosis and in others I think it’s helpful to hold it as a possibility while we treat signs and symptoms.
What Causes Dysautonomia?
Short answer, there is no short answer. Each case should be considered individually. But there are ways to organize our thinking around dysautonomia symptom presentations that can help us contextualize treatment. A symptom-based focus helps clients build a cognitive understanding which in itself creates stability in the presence of some pretty distressing symptomology.
The current literature discusses three types of dysautonomias:
Primary Dysautonomia: inherited or familial dysautonomia, pure autonomic failure, multiple system atrophy and some types of syncope (fainting due to sudden and brief decrease of blood flow to the brain).
Secondary Dysautonomia: Dysautonomia related to another disease process or in response to an infection or medication (i.e. folks who develop dysautonomia after getting COVID). [see panel]
Unknown/Idiopathic Dysautonomia: The cause or stimulating pathodynamic is unknown.
In my clinical experience the dysautonomiasis I see fall into the latter two categories. Sometimes, these categories seem to overlap. The dysautonomia may be caused by a “fill in the blank" event or other disease. It’s hard to know for sure.
Secondary Dysautonomia
Amyloidosis
Celiac disease
Charcot-Marie-Tooth disease
Chiari malformation
Crohn’s disease
Diabetes
Ehlers-Danlos syndrome
Ulcerative Colitis
Guillain-Barre syndrome
Human immunodeficiency virus (HIV)
Lambert-Eaton syndrome
Lupus
Lyme disease
Muscular sclerosis
Parkinson’s
Rheumatoid arthritis
Sarcoidosis
Sjogren’s syndrome
Vitamin B and E deficiencies
Case Example
I have a case that I am, for now, categorizing as a dysautonomia with an unknown cause. The main symptoms are:
Elevated heart rate
Anxiety
Heart palpitations
Temperature dysregulation (mostly hot and sweating all the time)
Dizziness
Vertigo/swirling - seated or standing
Light headed on standing (POTS like) but also light headed on sitting and laying down.
Heart rate spike when starting to feel relaxed
Fatigue
Nausea/loss of appetite.
Headaches/brain fog
Neck pain
This is a very typical symptom list that I suspect is familiar to you, whether clinically, personally, or with someone in one of your social circles.
This person is being treated by other professionals for POTS. However, the symptoms are a bit paradoxical for POTS and the treatments prescribed have not helped, even after giving several months to have an impact.
I am not disputing the POTS diagnosis. But the person’s system has made it clear that focusing there is not helpful in terms of symptom reduction. So, we pay attention and listen to the body and be curious about how else we may approach the case to give the person some relief.
How Do We Use Our Bodywork Skills to Help?
As bodyworkers we have so much to offer these folks. I have an informal list of strategies that I use to help those dealing with these multisystemic symptom presentations, regardless of cause.
Don’t assume a person’s symptoms are caused by trauma. Not everything that looks like the physiological response to trauma is trauma. The physiological disruptions caused by trauma look a lot like dysautonomia, both are symptom pictures of ANS dysregulation. However, conflating the two does a disservice to folks whose ANS is struggling because of something other than trauma.
Focus on the person’s experience and specific symptom picture: This is how we listen to the body. There are no protocols because each case is entirely different and unique.
Education is essential: I have done extensive training in working with trauma and HSD/EDS and both trainings emphasized education as one of the pillars of healing. Education helps create cognitive stability in the presence of overwhelming and confusing symptom experiences.
Reframe: Education and reframe go together. Your reframe will land more fully when it makes sense to the person based on the education you have done with them. Without a substantive foundation, a reframe can become a toxic positivity bypass.
Practitioner/Person Relationship: All of my training in both complex ANS cases and trauma share this predication on the relationship between you and your person.. Your relationship and connection matters - A LOT. Cultivate it. Build trust. Listen. Advocate. Validate. Educate. Stay steady. Take the long view but be responsive in the moment.
Be attentive in treatment: Be particularly and specifically attentive in treatment. I ask more questions and work more slowly and more deliberately in these cases. Less is more. I want to stay connected to how the nervous system is responding to treatment as best I can.
Techniques I most commonly use in these cases
In addition to focusing on all of the above, the bodywork techniques I use most in these cases are:
Visceral work: This goes right to the center of the physiology. The vagal system is intertwined with the viscera. Because the vagal system is 80% afferent fibers (sensing and sending back to the CNS) we can use this system to help the ANS recover a more healthy tone.
For folks who have studied visceral work, I use the sphincter treatment and diaphragm work (very gentle) as a beginning. Then follow what feels most relevant and helpful.
Remember, one the best vagal system treatments is connection. Your relationship matters. If your person feels connected to you, their system increases its potential to change.
Craniosacral Therapy: I find CST to be essential in these cases. The brain is the place where a lot of meaning making occurs. Often in the face of all of the physiological turmoil, the brain begins responding as if there is some other trauma present. Or, if the person has experienced trauma these two phenomena will merge in their system.
It is my experience that CST helps to change the brain state such that the system is interpreting signals differently. When the CNS is able to settle down, it gives the ANS some breathing room, which further supports the CNS calming down.
I can’t explain the exact mechanism by which this occurs, but based on years of clinical experience,I can tell you reliably that it does. As Gil Hedley teaches, we should hold our models (the stories about how our work works) loosely.
Myofascial Release: While MFR is not usually the main focus in these cases, I use it to support the above systems. However, see below – exceptions are the rule!
Let’s go back to the case example
The combined symptoms have a significant impact on this person’s quality of life and they are deeply frustrated, discouraged, and understandably frightened. They are also exerting a lot of energy to manage their care. In such cases I focus on:
Education + Reframing: This person has been understandably focused on getting an answer to what’s happening so that it can get treated and they can find some relief or resolution to the symptoms. I have emphasized paying attention to the dysautonomia while being attentive to the root cause, but not focused on it. There will be symptom changes without knowing the root cause when we pay attention to the body.
Treatment: The treatment combines visceral work and CST. In this case, the cervical tension is pronounced and the person identifies it as being related to their symptoms. So, I take that feedback as meaningful and incorporate myofascial work to support the CST work and the CST to support releasing the neck. In this case specifically, I have noticed/focused on:
Sphincters
Diaphragm
Gentle compressive release for the heart center combined with cervical myofascial work.
CST: we have noticed a significantly restricted sphenoid and are curious if some symptom change will correlate with the sphenoid picture changing?
They have a watch that tracks heart rate and we monitor this during treatment.
The jaw is tight/tense and we include work on the jaw with CST work.
Cervical MFR: interesting finding of very specific tension along the SCM, this is where the neurovascular bundle lives that contains the carotid sheath (vagus nerve, sympathetic trunk, internal jugular vein, internal carotid artery and lymph nodes). Treating this with gentle myofascial compression (think indirect technique) was helpful.
We also treated the posterior cervical myofascia, specifically the suboccipitals.
After our first treatment the person noted a symptom decrease that lasted almost two weeks. This was the most sustained relief they have experienced in quite some time. At the first visit the heart rate decreased from the low 100s to the low 70s. On their second treatment, the heart rate was in the mid 60s and remained there for the duration.
It’s possible this person is on the HSD spectrum or may have EDS as well, maybe not. We are keeping an open mind, staying curious, and treating what presents while paying attention to how the system responds. This may help clarify other diagnoses relevant in this case.
Where do we go from here?
These cases are always collaborative care cases. These folks need a team. We also need a team. A lot of what is happening in these cases is beyond our scope and training. And, some of it is directly in our wheelhouse. We can be instrumentally helpful when we are working in concert with a team of skilled, knowledgeable, and curious providers.
Take the long view. Look for change potential and amplify that for the person while also validating their struggles. It takes time to retrain a nervous system that has gotten out of whack, but change is possible.
Be curious and responsive to symptom shifts. We should be flexible in our approach. Just because a treatment worked in one visit, it may not work in the next. Listen to the person and pay attention to the specific symptom presentations. Let this guide how you approach each session.
Bodywork can be a pivotal component of an overall treatment plan.The more aware of the dynamics in these types of cases the more skillful we become in constructing treatments for these folks.