EDS / HSD Clinical Perspectives
May is Ehlers-Danlos Syndrome (EDS) awareness month. You can read an overview of EDS and its paired syndrome Hypermobility Spectrum Disorder here. I am three months into a training program through the Ehlers-Danlos Society’s ECHOs program. I have learned so much and feel humbled at what I was unaware of regarding the symptom pictures associated with these syndromes. It's more than bendy joints.
You are seeing folks with these syndromes weekly in your practice and they often are not getting the care that they need and deserve. Increasing awareness around these syndromes in our field is particularly important to address the care gap. These folks do not receive the care they need when interfacing with the conventional medical system and so find their way into the holistic medical field. Without a more complete understanding of the syndromes and their variable presentations we run the risk of also not caring for them in the ways that they deserve.
About the EDS ECHOs Program
For more information, go explore their resources and sign up on their website, be patient as their website is clunky. Search for the “Allied Healthcare Providers Track” and sign up for all the modules. They are affordable and will change your practice.
In Your Clinic
I have been seeing more of these patients than I realized - for years. It is humbling. As result of the ECHOs program I am able to read a new patient intake and have an idea of EDS/HSD may be part of the individual's experience and begin calibrating myself to their system before they come in for treatment.
Below is a list of some (not all) symptoms that folks may be experiencing as part of EDS/HSD.
Note: I am not saying these symptoms ARE EDS/HSD, but that they indicate it might be worth considering.
Some things to look out for include:
Changing pain patterns: i.e. pain in lots of places without known cause.
Pain since childhood or adolescence without known cause.
Dislocations
Individual seeing lots of specialists/providers and not gaining traction on their symptoms
Dysautonomia/POTS symptoms
Digestive problems
Vascular issues
Cognitive dysfunction
Nervous system issues such as tethered cord/Chiari malformation
Throat/swallowing issues
Mast Cell Activation Syndrome (MCAS)
The list can go on…
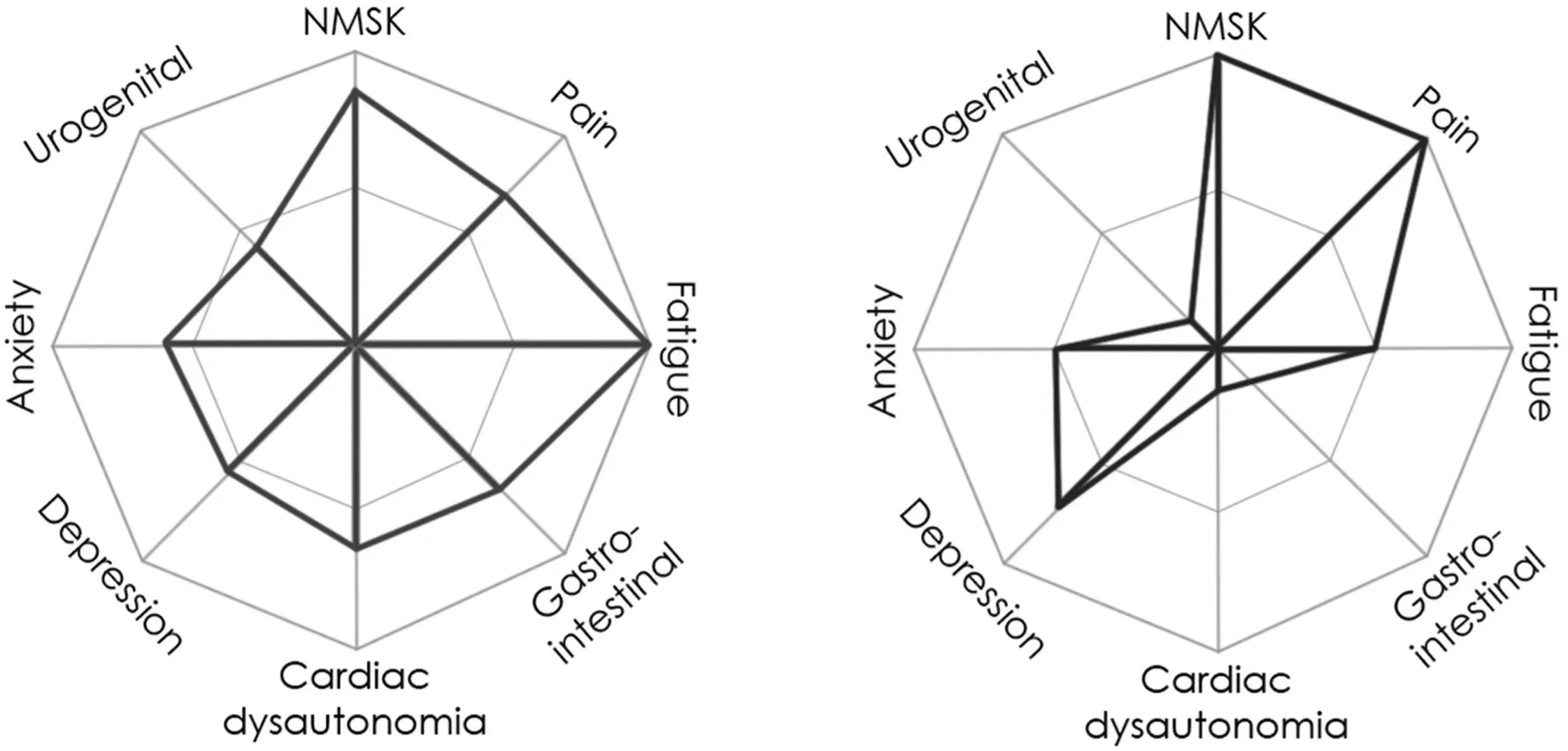
This can be a lot to try to parse out in a new patient visit. Sometimes, one grouping of symptoms is most active when the person comes to your office. Yet others can also be present. I love The Spider when it comes to complex symptom pictures.
From The Journal of Pediatrics: Clinical Practice
Volume 12, June 2024
The Spider - Multisystemic Visual Symptom Tool
When you look at this image I bet you can see specific folks in your case load. What you may not have been seeing is all of these symptoms unified under a single syndrome category. It is not possible for one provider to address all these symptoms so where and how do we fit in? This is how I am currently approaching this based on my skillsets.
Assess and Address (or not)
Whether it is a new patient or an existing patient, I ask myself does this look like an EDS/HSD picture (see Spider). If so, should I discuss it with the person? This is an important question. It could be helpful or it could create a negative spiral for the person, we have to be discerning.
I’ll bring it up if:
They are chasing a diagnosis and seeing a lot of providers or specialists and not getting help. It can help focus their care and support them in getting some much needed traction on at least some symptoms.
Is there a specific symptom that is louder than all the others that getting to the right provider could help with?
Will it create “cognitive stability” for them? Are they stressed and anxious about their symptoms and spiraling because of it? Discussing the possibility of EDS/HSD could be helpful.
I won’t bring it up if:
I don’t have good rapport yet.
They are already doing all the things that make sense and their symptoms are improving and their quality of life is good enough.
I determine that a diagnosis such as this will create significant mental emotional stress. If they are seeing me, I can support them without discussing the specifics of a diagnosis. We can always talk about it later. Time is a treatment, letting things breathe creates calm and stability.
Trauma Disclaimer:
One part of this symptom picture can have a significant impact on the nervous system. The symptoms fit a lot of what gets discussed under vagal system dysregulation. And, it’s true, the vagal system is involved, but why/how?
Our field currently has a strong reflex towards vagal system dysregulation = trauma. I think this is misguided and studying the realities of EDS/HSD has helped me expand my perspective significantly.
Folks can have vagal system dysregulation as a result of EDS and not have a history that indicates trauma. Full stop. It’s disrespectful to make assumptions about the folks that come to see us based on over-emphasing one thing in our mind, in this case an often narrow view of the “vagus nerve.”
For example, you may have a person who has MCAS as part of their EDS picture. Histamine dumps can happen in the early hours of the morning. The vagal system will totally trip out in the presence of all those histamines. The heart and respiratory rates will spike and it will “feel like” a panic attack. But the person will tell you they otherwise feel good enough emotionally. So, should we assume buried trauma or take them at their word and consider something else might be happening?
I think the latter.
How to Approach Treatment
Soft Skills
Cognitive stability is treatment: This means offering education and understanding are part of effective treatment. This is researched and presented within the ECHOs program.
Build a collaborative relationship with your clients and patients. These folks need allies, someone who will take the long walk with them through their symptoms.
Help them build the right care team for them. Collaborate with other providers.
Focus on achievable and reasonable goals. Have them set the goals and you support them. Symptom resolution is often impractical. Quality of life improvement can be in reach.
Use the Curable app with you people. This was discussed in our training and was viewed as helpful for folks.
There has been some concern expressed that discussing theories on pain is a form of gaslighting for folks with these conditions. The consensus from the Ehlers Danlos Society is that engaging with more understanding about the phenomenon of pain is empowering.
Myofascial/Joint/Nerve Pain
Listen to this episode of the Bendy Bodies podcast, it’s really helpful.
Treat from head to toe following your person's narrative of where they are experiencing pain, discomfort or things not working quite right.
There is often a somewhat stable pattern of discomfort/tension they experience. Working the whole path is so important.
Don’t fixate on addressing one specific area (see above).
Myofascial work is amazing for these folks. Be a bit more gentle and spend a little less time in each specific area. This really helps us improve our attentive tissue listening skills.
The ECHOs program also likes Fascial Counterstrain for these folks.
Including Craniosacral Therapy (CST) at the end of a session is helpful for integration and I think calms the nervous system. My instinct is that change in the tissue states can feel threatening to a system that might be in a protective state much of the time.
Central Nervous System/Dysautonomia /Tethered Cord Issues
Establish rapport and validate their knowledge of their situation. See above in soft skills. This is sooooooo important.
My go to for these symptom pictures is Craniosacral Therapy often combined with Visceral Techniques.
If you have studied Visceral Techniques you can likely treat the abdominal sphincters. I often start with contacting the diaphragm and treating the sphincters to help the nervous system receive other work.
Myofascial work combined with CST is helpful for folks with tethered cord. The tether is often in the lower thoracic or upper lumbar region. It can create a pull through the dura that creates pressures in the cranium and often at the base of the skulls and into the anterior throat.
Digestive + MCAS Digestion Related Symptoms
Visceral work combined with CST is excellent for these folks.
Diaphragm work is essential and I often repeat it throughout the session. As with the MFR above, be more gentle and do it for less time. Give the system space to find itself within your work.
I learned through work with a patient that jaw work with visceral work is really helpful. This was then confirmed in an ECHOs class.
MCAS can cause insomnia - see above on early morning histamine dumps. Sometimes, this work has helped mitigate this.
Throat Issues
This could also go under neurological but I made a specific category for it because the symptom picture is unique and would not immediately be classified as a CNS issue.
I have been seeing a significant increase in the numbers of folks coming in with “throat issues” over the last 7 or so years. For example:
Swallowing problems
Dysregulated breathing
Sleep apnea
It was discussed in a class on neurological manifestation of EDS that these issues can be caused by specific issues in the CNS along with these symptoms being related to dysautonomia.
There are an array of situations that might cause specific issues in the throat:
Intracranial hypertension
CSF leaks
A newish condition called Spiky-Leaky Syndrome
Chiari Malformation
These are general descriptions of situations I have experienced clinically that I imagine many of you are also seeing. I have found the ECHOs program to be deeply orienting for me in my clinical work and there is no way I could approximate the depth of that in a blog post. I hope you feel motivated to learn more about how you can help these folks with your skills and maybe develop your skills further to be of service to this population. I have found this to be gratifying work and appreciate the opportunity to use my skills to support folks with these symptoms, regardless of the underlying cause.
Related Reading
For more information on EDS/HSD, check out this article I wrote recently, Introduction to Ehlers-Danlos Syndromes (EDS) and Hypermobility Spectrum Disorders (HSD) in Our Practices.