The Vagal System in the Wild
How Theory and Techniques Meet in the Treatment Room
We have had a bit of vagal system extravaganza at MMI lately. I have been inspired by some dissection stuff during my class with Gil Hedley to re-look at vagal system anatomy. Dissection is messy business, and while we saw the vagus in the wild, as Gil likes to say, it was difficult to get the impressions of it that I wanted.
One incredible thing did happen. We were days into dissection and one of my dissection classmates called to me, “Michael, do you want to see the vagus nerve behind the heart?” I scurried over and was gobsmacked. She held the heart gently up from the posterior thoracic wall to show me that the vagus was not some singular nerve, nor a bilateral nerve innervating the heart from two sides. Rather, there was a spaghetti tangle of vagal fibers behind the heart as she lifted it up. The image was stunning, one I had never encountered in all my studies of the vagal system. We know the vagus goes to the heart but the physicality of this “going to” is hard to picture and not really communicated in vagal-related content.
I was re-inspired to explore the vagus as it exists in the body—not just in theory. After diving in, we had a great anatomy talk on the vagus in the throat, and the very next day, I had a patient experience that directly connected to what we had just studied. Read on for more about the vagal system in the wild.
Vagus nerve in relation to the glossopharyngeal, hypoglossal, & spinal accessory nerves
Vagal System in the Wild
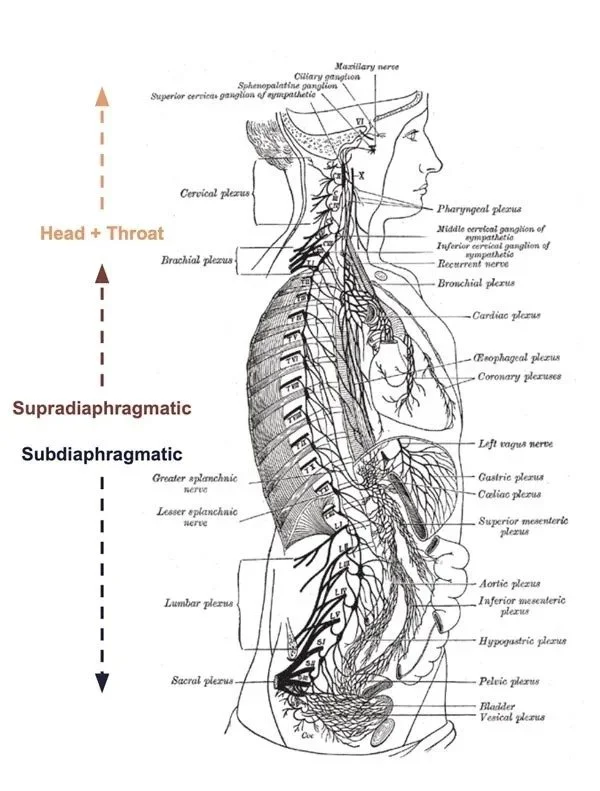
I have been in an ongoing process of disentangling myself from stories about the vagus nerve while still continuing to learn about this beguiling system. I have come around to thinking of the ‘vagal system’ rather than placing my focus on the ‘vagus nerve’ itself. When I see it as a system that involves the brain, sense organs, some of the muscles of expression, vocalization, swallowing, breathing, the organs of the thorax (heart and lungs), abdomen and pelvis, it becomes clinically useful and much more interesting. The “vagal system” reflects a body sensorium.
This vagal-system-sensorium is often involved in some of the weird symptom pictures folks come to us wanting help with. When we understand it as a system, it can serve as a map to orient us in the treatment room and offer guidance for how to approach treatment.
Case Example
The day after hosting an Anatomy Talk on the vagal system in the throat, my first patient presented a perfect example of using these ideas clinically.
The person was having a strange pain in their throat, the pain was lateral to the “throat stuff”, pharynx, larynx, thyroid, etc… and seemed oriented along, or at least near, the SCM. They reported that the pain often radiated under their jaw and towards the base of their tongue. They said sometimes, when the pain was particularly pronounced they would feel their carotid artery pulsating. All of it was disconcerting to this patient who also has health related anxiety.
Cognitive Stability as Treatment
Healthy cognition in the face of things we don’t understand is stabilizing to our system. Bodies are strange and are in and of themselves non-conformist. When bodies present sensations that we don’t fully comprehend and are painful or otherwise disruptive, it can be disorienting and produces all kinds of feelings. The unknown is often a source of anxiety for folks.
Understanding the vagal system and how it presents itself physically with sensation, symptom, and location is incredibly helpful for me clinically and why I like to share what I have learned.
I had just done a deep dive on this anatomy the night before and was able to offer my patient a lot of cognitive understanding.
We discussed:
The region of their symptoms was likely within the “carotid sheath” where the vagus nerve lives alongside the glossopharyngeal, hypoglossal and spinal accessory nerves, the internal and external carotid arteries and the internal jugular vein.
I shared how the nerves send out shoots—like plant shoots—to the muscles of the throat and the base of the tongue. This is where it helps to understand that the vagal system includes the glossopharyngeal and hypoglossal nerves and their related structures.
I explained some basic ideas about the vagal system, how it was intertwined with many of our stress responses, and asked if these symptoms occurred after any particularly stressful situation? They indicated, yes, the symptoms started after a very difficult work situation. The symptoms were often most pronounced when they were working at their desk.
We discussed that it sounded like they were having a very specific stress response in this area and it was impacting the muscles in their throat and tongue. They found all of this incredibly reassuring.
During our conversation they shared that they had gone to the internet in an attempt to understand what was happening and came away with increased fear. They were concerned that they might have “carotidynia” or “carotiditis”, inflammation of the carotid artery or carotid sheath.
I shared that the nerve ran through the sheath and the sheath was densely nested within the muscles of the anterior-lateral neck so pressure from tensing muscles could be why they are feeling their pulse. I asked if they felt the pulsing sensation all the time or just during pain episodes. They indicated only during pain episodes.
I validated for them that their concern was possible but was not my main hypothesis. I suggested that they go either to their doctor or urgent care and describe the symptoms and tell them that a HCP had suggested an ultrasound to rule out any issues in the carotid artery.
They felt further reassured that their fears were taken seriously andwere able to measure their fears against all the information we had discussed together.
By the time they got on the table we had done so much work together building cognitive stability around their symptoms and the fears related to their symptoms.
I wouldn’t have been able to provide such reassurance if I did not understand the anatomy and physiology of the vagal system so well (and was greatly aided by just having reviewed the actual anatomy!). One of the first things I learned as a bodyworker was the importance of recursive anatomy study; not for memorization, but for understanding and feeding the imagination so when we are faced with weird things in the clinic we can also orient ourselves in the clinical encounter by creating our own cognitive stability. When we can do this we are calm and grounded and that comes through to our people.
On the Table
This case is a perfect example of vagal-system thinking and treatment. I was not oriented to the nerve but to the places the nerve goes. Because most of the fibers are sensing and transmitting signals, I know I can contact the body to help it find calming sensations that the brain will recognize as calm.
When there is anxiety and high stress around a specific area of the body I don’t like to treat there first. It can be challenging for the person when they are already feeling challenged.
How I Approached the Treatment
We started with gentle work on the diaphragm. Helping the diaphragm relax and opening communication between the thoracic cavity and the abdomen is so helpful for so many things.
We then went to the abdomen and I treated the sphincters of the digestive system. These regions have dense arrays of vagal tissue and can be highly neuro-reflexogenic (fancy way to say they send info back to the brain).
I explained why I was working in the abdomen and it was an opportunity to reinforce the idea of the vagal-system both reflecting stress and being able to help create calm - via bodywork.
From there we went to an interesting hold where one hand sinks into the sternum, applying pressure to the heart center. The other hand cups the occiput and posterior upper cervicals. This is one of our students’ favorite holds to learn–it has so many different clinical applications. I used this technique to bring expansiveness to the heart center via the abundance of vagal fibers interpenetrating the heart and (as I saw in my dissection class with Gil Hedley) piled behind the organ. In this instance I was also using it to introduce some gentle myofascial work into the anterior-lateral neck.
Pericardium/heart resting on the diaphragm
Now we were ready to work more directly with the affected area. We did a combination of cervical myofascial work, gentle myofascial work for the jaw, intraoral work for the jaw and cranial work.
The work was profound for the patient and together we decided we had done enough in that area and they turned over face down and we did more myofascial work following tension patterns we are familiar with from previous work together. This work felt really good to the patient and helped them integrate some of the feelings that came up from the work we had done around the affected area.
It was a substantive session for this person. They received a lot of helpful information. Their body was able to express itself on the table and they could register and process that within the context of our conversation and not be hijacked by anxiety and fear. They had a specific referral to further allay their anxiety and they were in significantly less discomfort on all levels. All that in a 60 minute session.
Summary: Techniques as Lenses, Theory as Ground for Cognitive Stability
I think different techniques can serve as lenses into different body systems, even though we are always working with a single comprehensive system. In this instance the presentation oriented me towards the vagal system and I chose each technique according to that lens. I always ask myself, “How can I use what I know to address how I was understanding the situation?”
Key Points About the Treatment
Vagal system education and cognitive stability was the foundation of the treatment.
Myofascial-ish work for the diaphragm opened the center - breathing is stabilizing.
Using visceral techniques to further communicate through the vagal system created further grounding for the rest of the session.
Myofascial work with an eye to releasing tension around the jaw, throat and carotid sheath, without wanting to work too directly on the most affected area.
Craniosacral therapy to work with the CNS and facilitate some of the deep calm that can come from good Craniosacral Therapy.
Myofascial work for the posterior myofascial pathways on the same side as their symptoms and allow time and space for processing and integration.
In my experience, nerve based protocols are not nearly as effective as unpacking things for people and giving them solid information about their body, asking them questions that will help them connect that information to their lived experience, and then using all of that to guide how we approach work on the table. People deserve to be met in the fullness of their humanity in all of its weird, unpredictable and yet often understandable experiences and presentations. The more grounded we are in understanding the body the better able we are to create a container for them to feel met within.